The Science Behind Hormone-Linked Joint Pain
Research consistently shows:
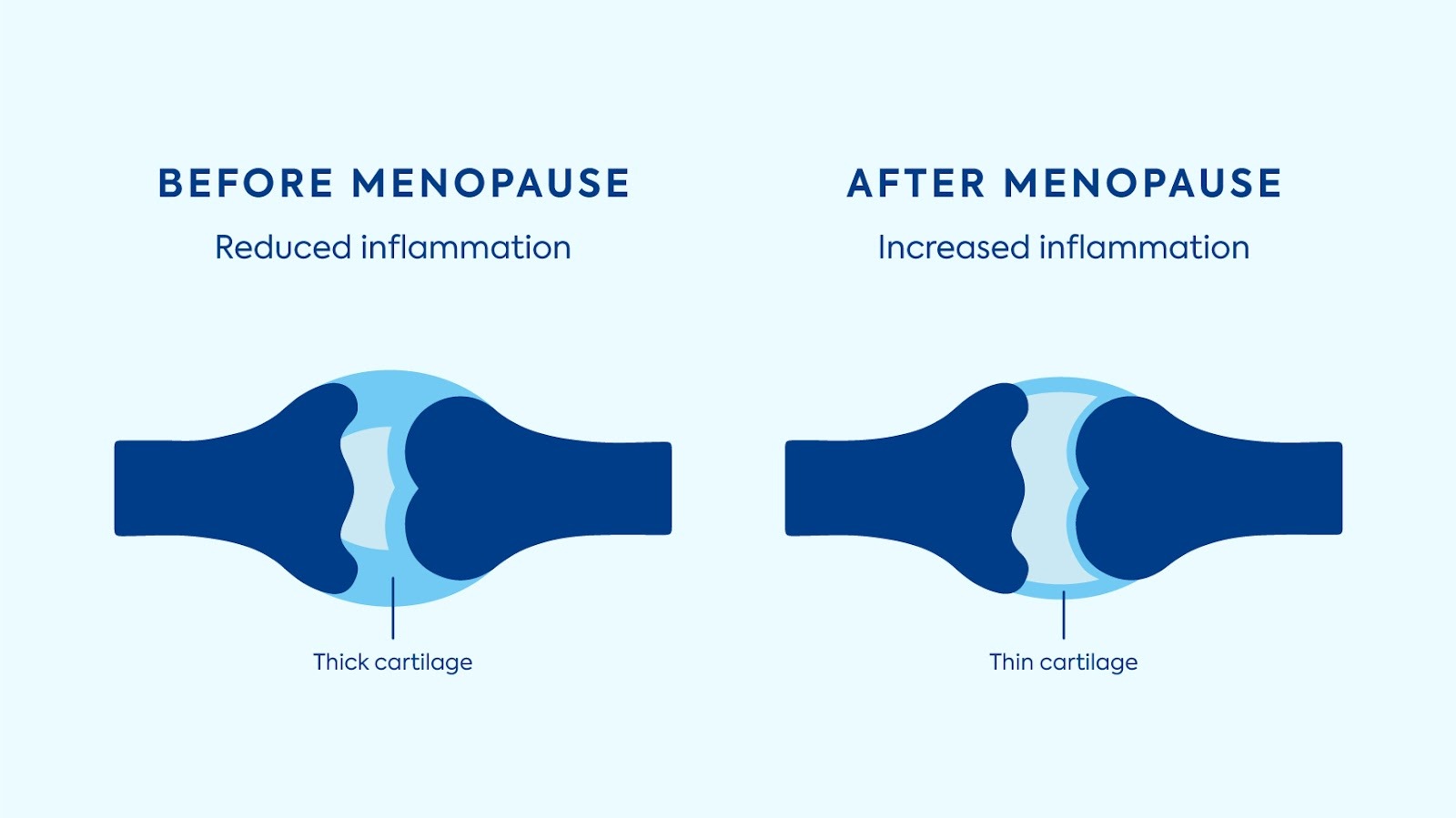
Estrogen Decline = Increased Inflammatory Signaling
As estrogen decreases, inflammatory cytokines rise, creating an environment where joints feel more sensitive [2].
Joint Pain Peaks in Late Perimenopause
This is the most volatile point of the hormonal transition. Symptoms often subside once hormone levels stabilize after menopause [1].
Cartilage and Connective Tissue Become Less Elastic
Lower estrogen reduces collagen production and joint lubrication, contributing to stiffness and slower recovery [3]. Women often pair hormone tracking with overall wellness monitoring using tools like the Diagnox Hydration Test Strips or Urinox-10, which can help identify other factors influencing inflammation.

How Hydration, Inflammation, and Lifestyle Influence Joint Pain
Several lifestyle factors make hormonal joint pain better, or worse.
Hydration
Even mild dehydration can worsen stiffness and slow joint lubrication.
Nutrition
Low-antioxidant diets and processed foods increase inflammation. Omega-3s, leafy greens, berries, and whole foods support joint health.
Movement
Low-impact movement like walking, yoga, swimming, and mobility work helps joints stay lubricated and reduces stiffness [6].
Stress
Stress hormones heighten inflammation, making joint discomfort feel worse.
When At-Home Testing Helps Most
You may benefit from testing if you:
• notice new joint stiffness
• feel changes in mobility
• have irregular cycles
• want to know if symptoms coincide with hormonal shifts
• are preparing to speak with a healthcare provider
• want to better understand your transition stage
The Diagnox Menopause Stage Indicator provides clarity in minutes.
Simple Ways to Support Joint Comfort Daily
• prioritize hydration
• incorporate gentle movement
• eat antioxidant-rich foods
• support sleep routine
• use heat or warm showers in the morning
• focus on recovery after activity
• track hormone changes with an at-home test
These steps don’t replace care from a healthcare provider but help support overall joint comfort during menopause.
Disclaimer
This article is for educational purposes only and does not diagnose or treat medical conditions. Always consult a healthcare provider for personalized guidance.





.webp)